
September 10, 2024
Pee Urinary Incontinence A Summary

Impacts Of Estrogen With And Without Progestin On Urinary System Incontinence Geriatrics Jama From the age of puberty to menopause, hormone variations can influence the stamina and function of the pelvic floor muscle mass, commonly bring about urinary issues such as stress and anxiety urinary incontinence (SUI). A big part of this is due to pregnancy, giving birth and menopause. Each of these events in a lady's life can lead to bladder control problems. Maternity can be a temporary source of urinary incontinence and the bladder control concerns generally get better after the infant is birthed. Some women experience urinary incontinence after delivery due to the stress childbirth takes on the pelvic floor muscle mass. When these muscular tissues are compromised, you're more probable to experience leak concerns. Hormonal agent therapy (estrogen) in postmenopausal ladies minimizes urinary system frequency and dysuria and blood circulation of bladder cells boosts and leads to enhance the stamina of muscles around the urethra [44] Steroid hormonal agents in addition to ecological effects in the urinary system tract have a main function in the neural control of peeing procedure. Nonetheless, the specific device of this activity is unknown, however the existence of both sorts of estrogen receptors in the mind cortex, limbic system, the hippocampus and the brain has been verified [36]
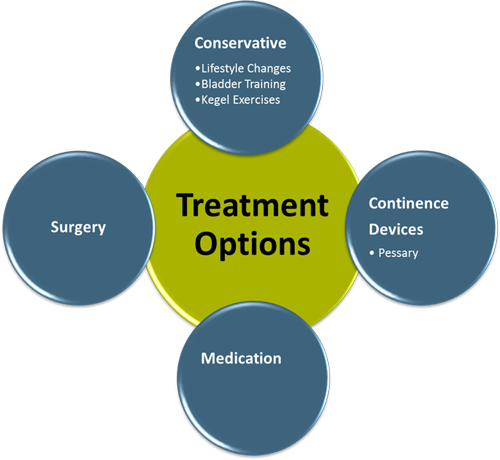
Treatments
Because of the placement and Bladder infection feature of steroids in the urinary system system, the use of replaced hormone treatment in menopause has actually long brought in the focus of scientists and suppliers of health care in this field. In females without urethral hypermobility, the urethra is stabilized during stress by three interrelated mechanisms. One device is reflex, or volunteer, closure of the pelvic flooring. Tightening of the levator rectum complicated elevates the proximal urethra and bladder neck, tightens up undamaged connective cells supports, and elevates the perineal body, which may act as a urethral backstop. If you're experiencing urinary incontinence during your duration or your cycle, it can transform your quality of life.News From Mayo Facility
These drugs all have the possible to trigger uneasyness, tachycardia and hypertension. Ephedrine is administered at a dose of 4 mg/kg every 8 to 12 hours. Several huge breed dogs might be started on 25 mg every 8 hours, boosting the dose to 50 mg if there is no scientific action at the reduced dosage. Phenylpropanolamine has the very same strength and pharmacologic homes as ephedrine but seems to trigger much less central nerves stimulation. The advised dosage is 1.5 to 2.0 mg/kg twice daily to 3 times daily. Pseudoephedrine is similar to ephedrine and phenylpropanolamine.What Are My Hormonal Agent Therapy Options?
Preserving a healthy body weight can likewise help with bladder control. Talk to your healthcare provider about the most effective methods to maintain strong pelvic floor muscles throughout your life. Incompetence of the urethral sphincter device (urethral smooth/striated muscular tissue, connective cells) might arise from nonneurogenic illness (bladder, urethra, prostate gland) or neurogenic causes.- Double-contrast cystography may be indicated for complete visualization of the urinary bladder and recognition of urinary bladder sores.
- In biofeedback, a cord is linked to an electrical patch over your bladder and urethral muscles.
- Advise urinary incontinence is more widespread after the menopause, and the top occurrence of stress urinary incontinence takes place around the moment of the menopause.
- These hormonal changes can influence bladder feature and urinary system behaviors, showing up as urinary system signs such as raised regularity, seriousness, or leak.
- Stress urinary incontinence establishes when task places raised stress on your bladder.
What hormonal agent keeps you from peeing?
Social Links