
September 1, 2024
Urine Urinary Incontinence An Introduction
Impacts Of Estrogen With And Without Progestin On Urinary Incontinence Geriatrics Jama [23] is titled the relationship in between menopause and urinary system incontinence that women with urinary system incontinence than those who did not have, dramatically had greater BMI [24] Healthcare professionals need to consider urinary system incontinence a medical concern and develop proper diagnostic skills. They need to have the ability to determine and manage any type of appropriate modifiable aspects that can minimize the problem. 1) Urodynamic test where stress of bladder and urethra are determined. It does not seem that the initial Continence-preserving workouts cause of dystrophy or carcinoma of external genitalia is estrogen deprivation. Hit to genital might be in charge of about 15 percent of blood loss after menopause, and on the various other hand, the occurrence of Vaginitis throughout the years after menopause boosts. Some think that certain kids create a pattern of not unwinding the pelvic flooring while nullifying. Sometimes, this can be traced back to an infection or some other noxious stimuli. A vicious circle of pelvic flooring spasm, constipation, and urinary system retention can develop.About Mayo Center
The treatment causing reduced testosterone degrees might compromise the pelvic flooring muscle mass, bring about UI. Consequently, treatments such as pelvic exercises may be required in handling UI if you are obtaining ADT. Also quit the flow of urine in midstream pee creates to enhance the pelvic floor muscles.News From Mayo Clinic
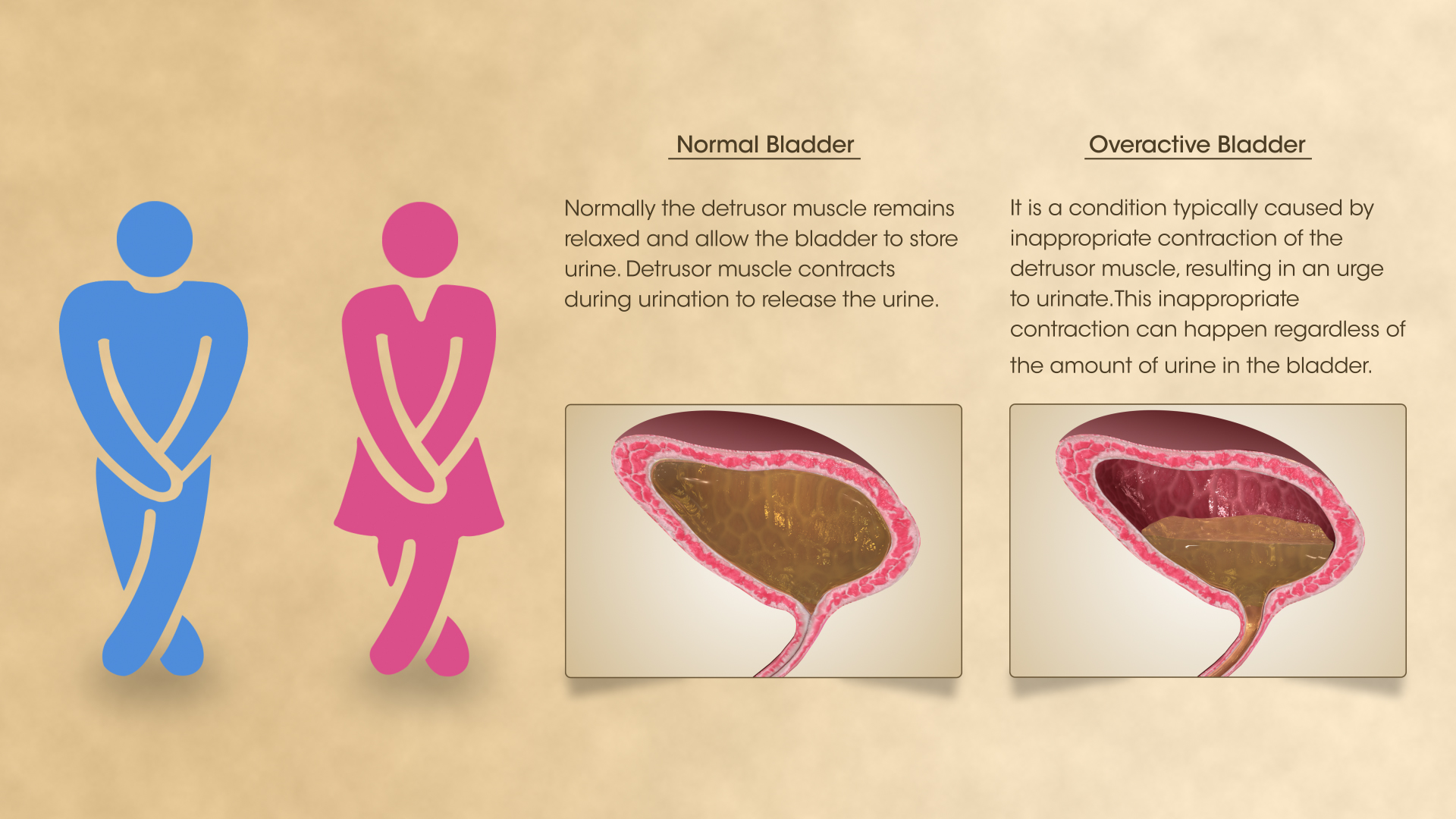
Your bladder resembles a storage tank-- when the bladder is full, the brain sends out a signal that it's time to urinate. Pee after that leaves the bladder when a muscle opens up (sphincter), allowing the urine to move freely out of the body with the urethra. It is very important to determine the type of urinary system incontinence that you have, and your signs usually tell your medical professional which kind you have.Overflow Urinary Incontinence Pathophysiology
Discover if you qualify to get urinary incontinence supplies free via your insurance policy at the bottom of the web page. A person needs to talk to a doctor if they have any type of issues they might have low estrogen or if they are experiencing bladder signs. Reduced estrogen can additionally influence people outside of menopause, especially after delivering or during breastfeeding. As lots of as 15% of premenopausal females may have GSM-like symptoms consequently. Nonetheless, they can additionally drop during various other stages of life, such as after delivering or while breastfeeding.- Double-contrast cystography may be indicated for full visualization of the urinary system bladder and recognition of urinary system bladder sores.
- Endocervix glandular cells activity throughout menopause and ultimately the quantity of mucin reduces that this triggers to genital dryness that develops as a major issue in postmenopausal women.
- Urge urinary incontinence is more common after the menopause, and the peak prevalence of tension incontinence occurs around the moment of the menopause.
- These hormonal changes can influence bladder function and urinary habits, materializing as urinary system signs such as increased frequency, seriousness, or leakage.
- Stress urinary incontinence develops when activity puts enhanced stress on your bladder.
How to cleanse your bladder normally?

Social Links