September 6, 2024
Impact Of Conjugated Estrogen In Anxiety Urinary Incontinence In Women With Menopause
Management Of Urinary System Incontinence In Postmenopausal Females: An Emas Medical Rehabilitation Guide Distinguishing between voluntary and uncontrolled peeing is basic to the diagnostic strategy. Three kinds of lesion of disintegration, ectropion and cervical lesions in post-me- nopause is seen a lot more. Endocervix glandular cells activity throughout menopause and ultimately the amount of mucin lowers that this triggers to genital dryness that emerges as a major complaint in postmenopausal ladies. Later on, in a subgroup of these people, myopathic adjustments may happen in the bladder that make the spread of abnormally created contractile signals more efficient and harder to subdue voluntarily. These connective-tissue parts form the passive supports to the urethra and bladder neck. Throughout times of increased intra-abdominal stress, if these supports are undamaged, they increase the encouraging impact of muscular closure of the pelvic flooring. INNOVO's special Multipath ™ Modern technology makes certain optimal muscular tissue interaction and efficacy, delivering targeted stimulation to the pelvic flooring muscle mass without the need for invasive probes or hand-operated treatment.Impulse Incontinence Pathophysiology
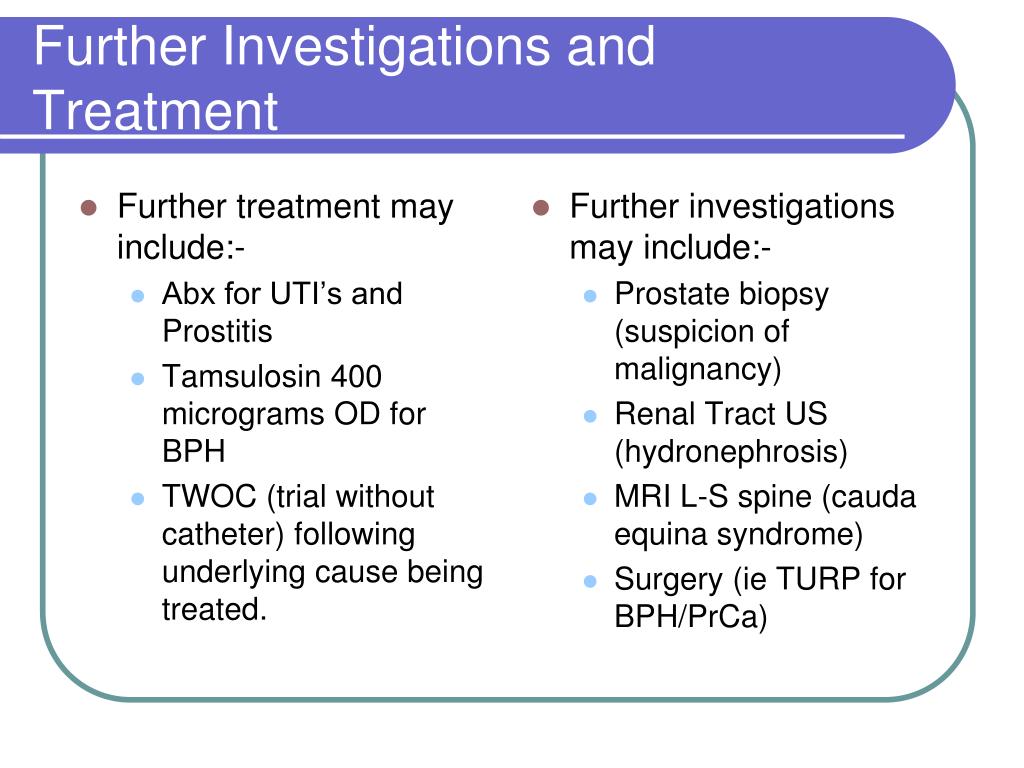
Because of the setting and feature of steroids in the urinary system, making use of replaced hormonal agent therapy in menopause has actually long brought in the focus of scientists and service providers of health care in this field. In ladies without urethral hypermobility, the urethra is stabilized throughout tension by 3 related mechanisms. One system is response, or volunteer, closure of the pelvic floor. Tightening of the levator rectum facility elevates the proximal urethra and bladder neck, tightens up intact connective tissue sustains, and raises the perineal body, which might work as a urethral backstop. If you're experiencing incontinence during your duration or your cycle, it can transform your quality of life.How Is Urinary Incontinence Dealt With?
Urethral inexperience generally leads to recurring urinary system incontinence, generally at rest. Hormone treatment (estrogen) in postmenopausal females minimizes urinary frequency which causes increase in the toughness of muscles around the bladder. Althoughbasic science in this area is limited, a current placebo-controlled, randomizedclinical test of estrogen alone sheds light on this problem. Urethral closureis depending on the integrated activity of the suburethral vaginal wall surface, thepubourethral tendons, the pubococcygeus muscular tissues, and the paraurethral connectivetissues. As you age, the muscles that support your pelvic body organs can damage. This means that your bladder and urethra have less assistance-- often leading to urine leak.Comprehending Stress And Anxiety Urinary Incontinence (sui)
Learn if you certify to get incontinence materials totally free with your insurance policy at the end of the page. A person must speak to a doctor if they have any kind of problems they might have reduced estrogen or if they are experiencing bladder symptoms. Low estrogen can likewise affect individuals outside of menopause, specifically after delivering or throughout breastfeeding. As several as 15% of premenopausal females may have GSM-like signs and symptoms consequently. Nonetheless, they can also go down during other phases of life, such as after delivering or while breastfeeding.- Double-contrast cystography may be indicated for complete visualization of the urinary bladder and recognition of urinary bladder lesions.
- In biofeedback, a wire is linked to an electrical spot over your bladder and urethral muscles.
- Advise urinary system incontinence is much more common after the menopause, and the optimal prevalence of tension incontinence occurs around the time of the menopause.
- These hormonal changes can influence bladder function and urinary routines, materializing as urinary symptoms such as enhanced regularity, urgency, or leakage.
- Anxiety incontinence establishes when task places enhanced stress on your bladder.
Which hormone is responsible for bladder?

Social Links