
September 3, 2024
The Results Of Hormones On Urinary System Incontinence In Postmenopausal Women
Urinary Incontinence: Leak, Triggers, Diagnosis, Therapy & Prevention The study was reviewedand authorized by the human topics evaluate committees at each participatinginstitution, and all participants offered written informed approval. For people with a decompensated bladder that does not empty well, the postvoid residual pee can result in overgrowth of bacteria and succeeding urinary system tract infection (UTI). Anxiety incontinence influences 15-60% of ladies-- both young and old people. Greater than 25% of nulliparous young college professional athletes experience stress and anxiety incontinence when taking part in sporting activities. Patients with a neurogenic disorder such as myelomeningocele may have an open bladder neck that leads to extreme intrinsic sphincter deficiency and urinary system loss.
- Some common side effects of mirabegron include nausea, looseness of the bowels, irregularity, dizziness and frustration.
- In addition, prolapse of the anterior genital wall can impact bladder draining.
- Private incontinence problems, therapy and recuperation times might differ.
- As you age, your estrogen degrees decline significantly-- especially throughout menopause.
How Is Urinary Incontinence Detected?
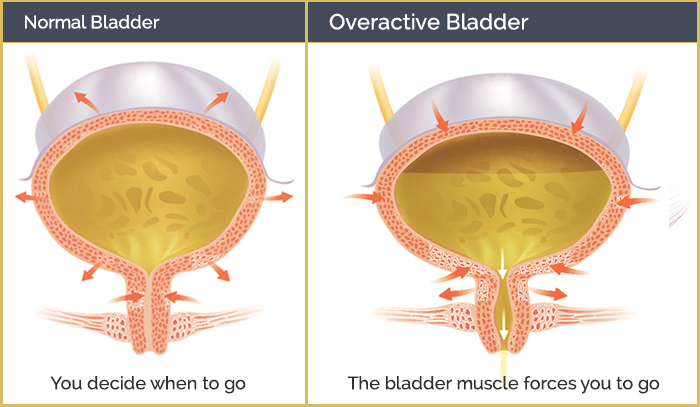
A few examples of this are coughing, sneezing, chuckling, or exercising. In these instances, weak pelvic flooring muscular tissues are incapable to offer correct support for your bladder, so pee might leak out. According to a study released in the Continue reading Journal of American Urogynecologic Society, over 60% of adult women in the US suffer from this humiliating problem. It is referred to as urinary system incontinence (UI) and is an usual postmenopausal disorder. Although mobile, the anterior urethral wall has been observed to stop moving, as if tethered, while the posterior wall surface remained to rotate and come down. Possibly, the pubourethral tendons apprehension rotational movement of the anterior wall surface but not the posterior wall. The resulting separation of the former and posterior urethral wall surfaces could open up the proximal urethral lumen, therefore enabling or adding to stress and anxiety incontinence. For recognizing urinary incontinence, the relevant anatomy of the lower urinary system tract comprises the urethra and bladder. Go to Urinary System Urinary Incontinence Appropriate Anatomy to find out more on this topic. Urinary incontinence in women is not a recent medical and social phenomenon, yet the loved one relevance attributed to urinary system incontinence as a clinical trouble is increasing.Comprehending The Link Between Bladder Control & Your Duration: Suggestions For Women
What are the 4 hormonal agents influencing the urinary system?
Incontinence can take place for several factors, consisting of urinary system tract infections, genital infection or inflammation, or irregularity. Menstruation adjustments. There are lots of factors your monthly duration can change, yet hormone imbalance frequently plays a role.Hair problems. Hormonal agents affect hair's natural cycle
Social Links