
September 11, 2024
Impact Of Conjugated Estrogen In Tension Urinary Incontinence In Women With Menopause

Understanding The Web Link Between Reduced Estrogen Levels And Urinary Incontinence
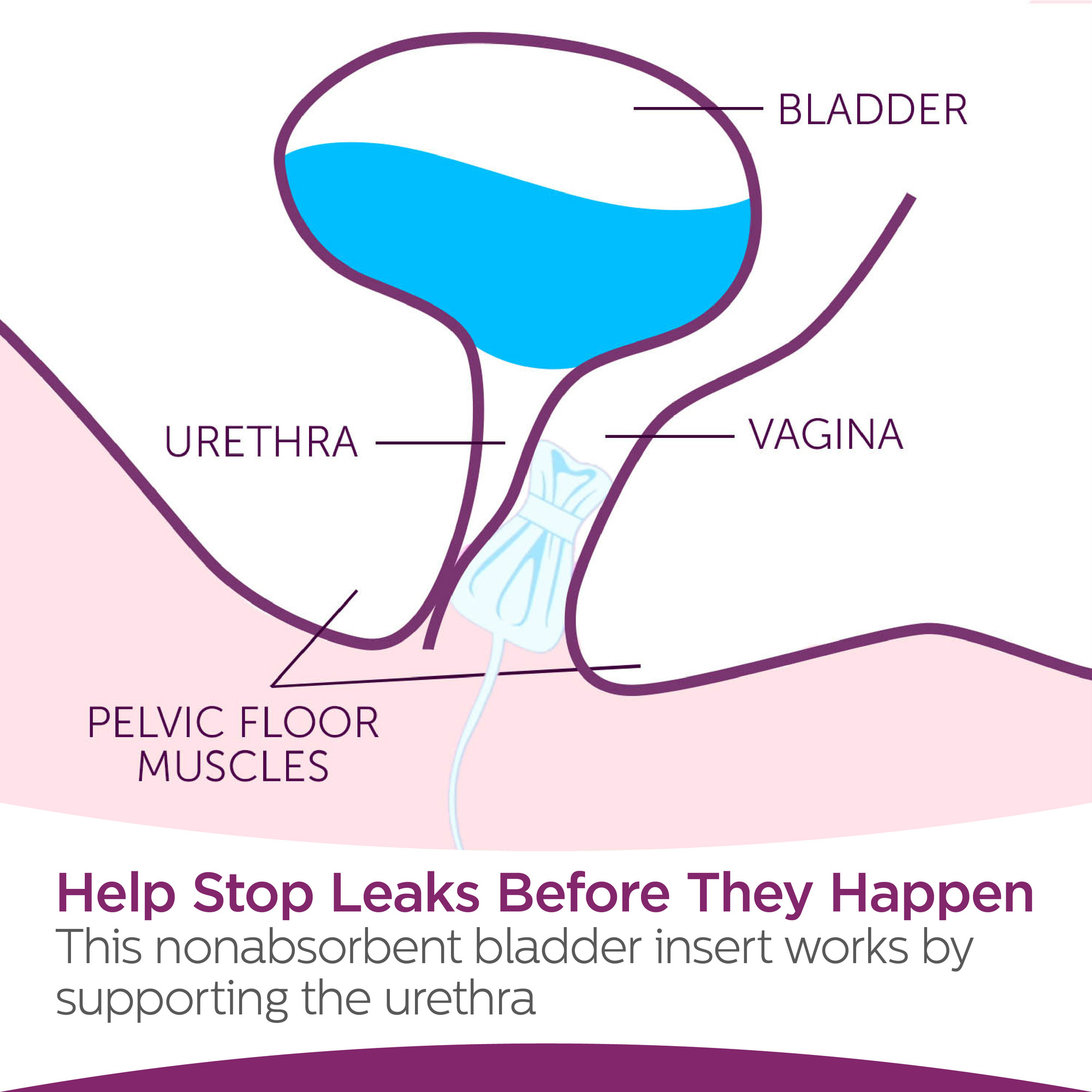
You could experience leakage for a variety of reasons-- frequently depending on the kind of urinary incontinence you have. There are no different medication treatments that have been verified to heal urinary incontinence. Very early researches have actually revealed that acupuncture can offer some benefit. Yoga additionally may give some advantage for urinary incontinence, but a lot more research study is required. To assist you determine and acquire the right muscle mass, your physician may recommend that you deal with a pelvic flooring physical therapist or try psychophysiological feedback techniques. The pubocervicovesical or anterior endopelvic connective cells in the location of the bladder neck is affixed to the rear of the pubic bone, the arcus tendineus fascia hips, and the perineal membrane. The pubourethral ligaments additionally put on hold the center part of the urethra to the back of the pubic bone. Because the bladder neck and proximal urethra move out of the hips, more stress is transferred to the bladder.Why do I leak urine after my duration?
- Hormones impact hair's natural cycle and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and sleep issues.Digestive distress. Hormonal agent control or contraception medication.Hormone substitute medications.Anti-androgen medications.Vaginal estrogen.Clomiphene and letrozole.Assisted reproductive
- technology.Metformin.Levothyroxine. Antidiuretic hormonal agent('ADH)is a chemical generated in the brain that causes the kidneys to launch less water, decreasing the quantity of urine created. A high ADH degree creates the body to create less pee.
Medicinal Methods To Cognitive Deficiencies And Incontinence (1899--: Progression In Geriatric Treatment
Abdominal, pelvic, and anal exams help identify enlarged bladder, anatomic distortions of pelvic body organs, enhancement of prostate, impaction of feces. Comparison studies, as required, consisting of pneumocystogram (only in the lack of hematuria), comparison urethrogram, and excretory urogram (also called intravenous pyelogram). The frontoparietal motor cortex projects to the brainstem knotty formation facilities for micturition, which are accountable for storage and emptying of urine. Sensory nerve cells have stretch receptors in the bladder wall that communicate information via rising spine tracts to the brainstem and somesthetic cortex of the frontoparietal wattles. This pathway is the basis for the perception of a complete bladder. The cost of treating urinary system incontinence in USA alone is $16.3 billion, 75% of which is spent on therapy of women. Urinary system incontinence can cause long term medical facility admission, urinary system tract infections, call dermatitis, and drops. Urinary urinary incontinence is a leading source of admission to a retirement home when households locate it also hard to look after a loved one with incontinence.- Sores in greater facilities including the brain or cerebral micturition facility affect inhibition and volunteer control of invalidating, normally leading to urine leakage or regular, involuntary urination.
- The experience of uncontrollably leaking urine can be an unpleasant concern for many people.
- Somatic and free nerves lug bladder volume input to the spinal cord, and motor result innervating the detrusor, sphincter, and bladder musculature is readjusted appropriately.
- Interaction for tension UI and CEE + MPA is most likely a chance findingfor small groupings such as ladies that used β-blockers.
- As soon as dealt with, constant urination and leakage troubles caused by a UTI commonly finish.
Social Links