September 8, 2024
Menopause And Urinary System Incontinence
Menopause And Urinary Incontinence Hormone Replacement Therapy (HRT) is a form of treatment that entails the management of hormonal agents, specifically estrogen, progestin (a kind of progesterone), or both. A woman's body quits generating these hormonal agents after menopause, resulting in conditions such as urinary system incontinence. Reintroducing the hormonal agents in different kinds, https://Achievable-wellness.b-cdn.net/Achievable-wellness/bladder-control/coping-behaviors-usual-in-ladies-with-overactive.html consisting of tablets, spots, creams, and vaginal rings, can help turn around the impacts of these conditions. Urinary system incontinence (UI) is additionally referred to as "loss of bladder control" or "spontaneous urinary leakage." Countless females experience it, and the regularity of UI has a tendency to increase as you age. Grown-up baby diapers are one of the most effective remedies for women to manage this important transition and remain active regardless of their estrogen deficiency. One of one of the most effective treatment approaches is hormone substitute treatment (HRT). HRT supplements your body with the estrogen it no longer makes, assisting to restore hormonal balance, boosting urinary system wellness, and lowering urinary system incontinence signs. Prompt incontinence, or overactive bladder, occurs when you really feel an abrupt and extreme impulse to pee, adhered to by involuntary urine leakage. Low estrogen degrees can irritate your bladder muscular tissues, resulting in enhanced level of sensitivity and overactive bladder.Comprehending The Link Between Reduced Estrogen Degrees And Urinary System Incontinence
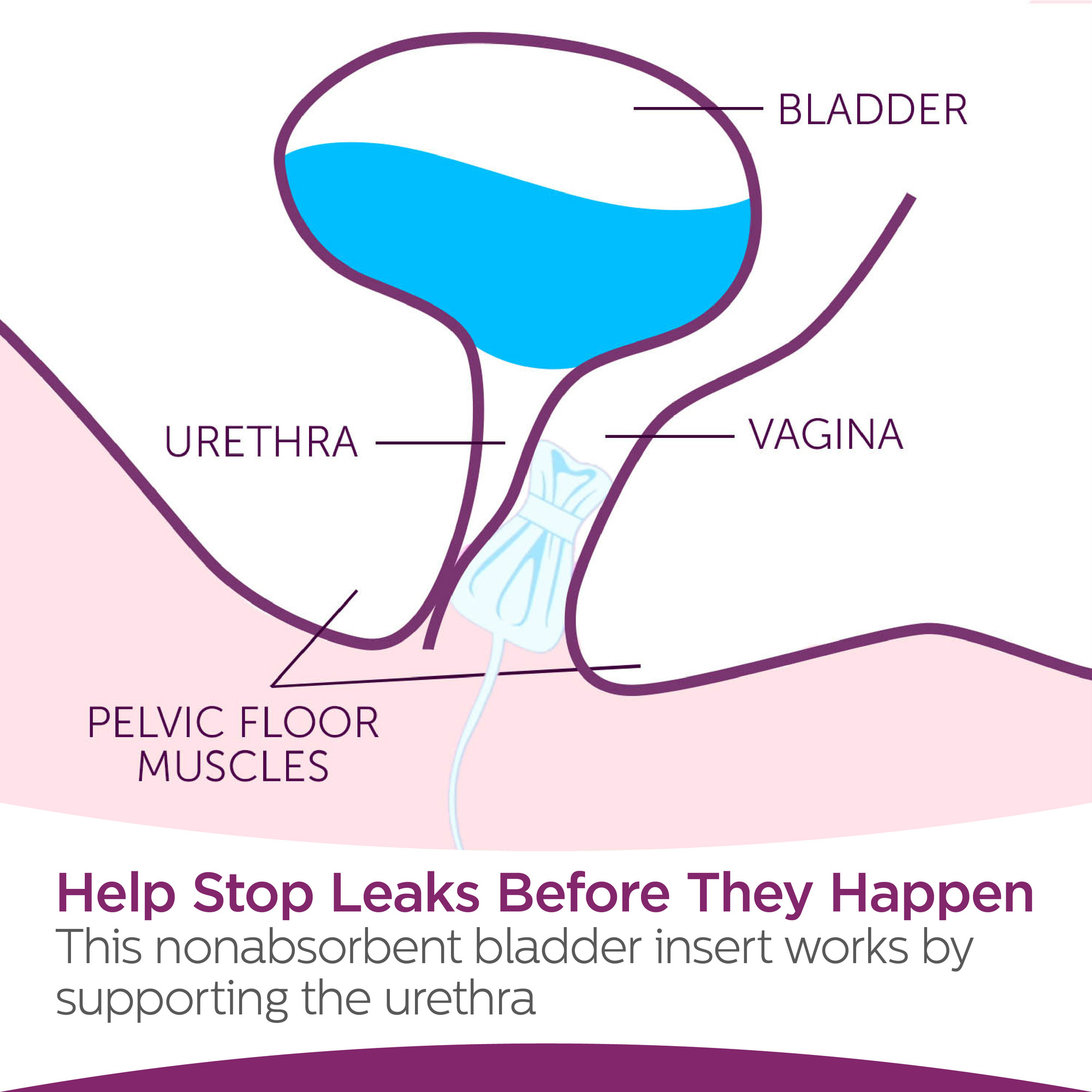
On top of that, the individual relearns just how to manage the bladder and strengthen the entailed muscular tissues. Urinary system bladder hypocontractility or poor lodging of pee throughout storage might bring about frequent leak of little quantities of pee. Dysfunction might be brought on by urinary system tract infection, persistent inflammatory disorders, neoplastic sores, outside compression, and persistent partial electrical outlet obstruction.Factors To Pick Laparoscopy Over Conventional Treatment
These medications all have the possible to create uneasyness, tachycardia and high blood pressure. Ephedrine is provided at a dosage of 4 mg/kg every 8 to 12 hours. Numerous huge breed pet dogs might be begun on 25 mg every 8 hours, increasing the dose to 50 mg if there is no medical reaction at the reduced dosage. Phenylpropanolamine has the very same effectiveness and pharmacologic residential properties as ephedrine but seems to create much less main nerve system excitement. The suggested dosage is 1.5 to 2.0 mg/kg two times daily to 3 times daily. Pseudoephedrine is similar to ephedrine and phenylpropanolamine.Therapy For Low Estrogen Bladder Signs
It likewise helps maintain your bladder and urethra healthy and functioning properly. They may no more have the ability to control your bladder as they did before. As your estrogen levels remain to drop throughout and after menopause, your UI signs and symptoms might worsen. Estrogens, typically in the kind of diethylstilbestrol, are administered to spayed females.- Low estrogen can cause bladder signs by thinning the cells that lines the vaginal canal.
- They might suggest Mirabegron (Myrbetriq), an unique type of medication called a beta-3 adrenergic receptor agonist, to raise the amount of pee your bladder can hold.
- Medical diagnosis would be based on discovering urinary retention and direct proof of the blockage (e.g., urolith).
- Any task-- flexing over, jumping, coughing or sneezing, for example-- may press the bladder.
- The aging of the genitourinary system by high levels of circulating estrogen is readjusted.
What hormone keeps you from peeing?
Social Links