
September 3, 2024
Menopause And Urinary Incontinence
Therapy
Can hormone inequality impact your bladder?

Neurologic Causes
Hormone Substitute Treatment (HRT) is a form of treatment that involves the management of hormones, especially estrogen, progestin (a form of progesterone), or both. A woman's body stops generating these hormonal agents after menopause, bring about problems such as urinary incontinence. Reestablishing the hormones in numerous forms, consisting of tablets, spots, creams, and vaginal rings, can aid reverse the effects of these disorders. Urinary urinary incontinence (UI) is additionally known as "loss of bladder control" or "uncontrolled urinary system leak." Millions of ladies experience it, and the regularity of UI often tends to enhance as you get older. If guided to pursue surgical treatment by your medical professional, prompt activity is suggested, as waiting might decrease the effectiveness of surgical therapy. The viewpoints expressed in individual reviews are by patients only; they are not qualified medical professionals. These point of views need to not be relied upon as, or instead of, the clinical advice of a qualified physician, and so on. Urinary incontinence is a common condition influencing several individuals, especially postmenopausal females. In addition, the client relearns exactly how to control the bladder and enhance the entailed muscles. Urinary bladder hypocontractility or bad holiday accommodation of urine during storage space may lead to constant leak of tiny quantities of urine. Disorder may be triggered by urinary system tract infection, persistent inflammatory problems, neoplastic lesions, outside compression, and chronic partial electrical outlet blockage. Signs and symptoms of overactive bladder or prompt urinary incontinence in the absence of neurologic causes are understood merely as detrusor overactivity. Furthermore, much research has actually been performed to bolster the understanding of the neurophysiology of the bladder, urethra, and pelvic floor. Ultimately, interest in the diagnosis and therapy of urinary incontinence is ongoing.- The increasing degrees of estrogen, together with the stress placed by the growing unborn child on the bladder muscular tissues, results in urinary incontinence.
- If you have a chronic condition like diabetic issues or several sclerosis, you might have incontinence for a. long period of time.
- The recommended dosage is 1.5 to 2.0 mg/kg twice daily to 3 times daily.
- Often it is the very first and only symptom of an urinary system system infection.
Qualifying For Free Urinary System Incontinence Products
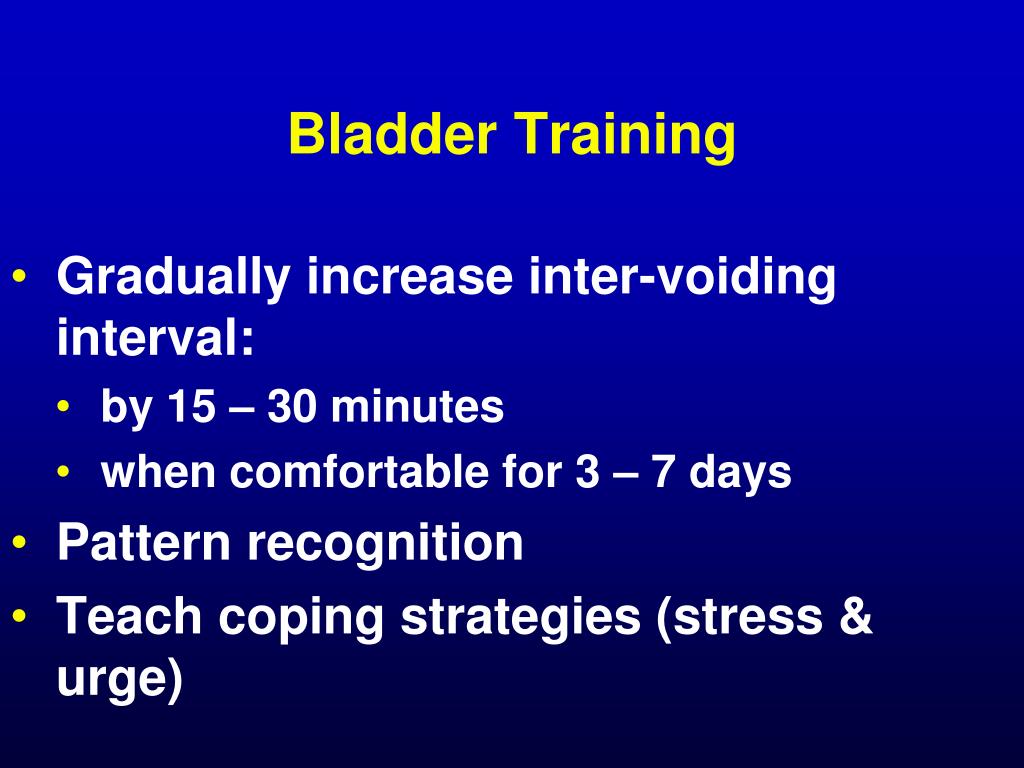
One of the treatments you might be suggested for managing UI is hormonal therapy. Along with dealing with urinary system incontinence, this therapy alleviates a number of other postmenopausal conditions, such as genital dryness, evening sweats, and hot flashes. You can experience UI throughout your life, yet the majority of episodes are the result of stress or stress and anxiety on the muscles that assist you hold or pass urine. Hormone changes can also impact your muscular tissue strength in the pelvic area. As a result, UI is more usual in women who are expectant, Click for source delivering, or going through menopause. The individual is trained to empty the bladder at a particular time of day.Social Links