
September 10, 2024
Incontinence

Ambulatory Urodynamics
Urethral pressure profilometry can additionally be accomplished by using water-perfused catheters. Every individual ought to go through pee dipstick testing to rule out urinary system infection and determine any tiny haematuria that may call for additional examination. For instance, it is typically more effective to define individuals of Oriental ancestry according to their country or local location of origin (eg, Cambodian, Chinese, Indian, Japanese, Oriental, Sri Lankan, East Asian, Southeast Asian). No restrictions were positioned on the publication timeframe or the study country, yet only English language research studies were consisted of. Twenty-six financial analyses were included, of which 13 were model-based evaluations. Surgical therapies examined most regularly were mid-urethral slings and open and laparoscopic colposuspension. There were some distinctions in the technical techniques taken, including differences in type of economic analysis, perspective, time horizon, kinds of source use, and expenses and results that were consisted of in the evaluation.- For ladies with light UI, disposable insert pads (within washable pouch trousers) were most efficient.
- In such instances, the categories included in "various other" teams need to be specified and reported.
- OnabotulinumtoxinA intersphincteric injections in external striated urethral sphincter may boost invalidating in patients with DU by reducing electrical outlet resistance and lowering the guarding reflex.
What is the issue with urinary incontinence?
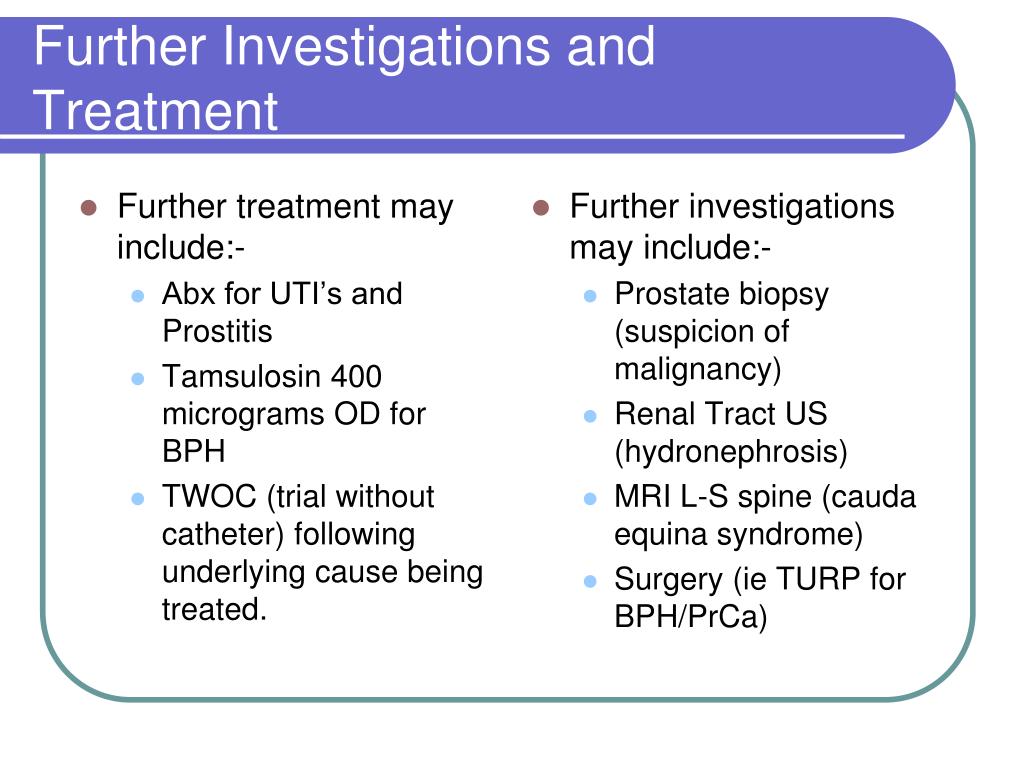
Medical Treatment
Treatment of women DU includes techniques to make sure bladder water drainage, rise bladder contraction, lower urethral resistance, or a combination of the two [474] The administration objectives for UAB are to improve signs and symptoms and QoL, to reduce the danger of issues, and to determine scenarios where treatments may not be appropriate. A Cochrane evaluation contrasting PFMT with no or sham therapy included 31 RCTs from fourteen nations, but there was only one study consisting of women with MUI and one with UUI and none reported information on remedy, enhancement, or variety of episodes of these subgroups [316] Blended urinary system incontinence is tough to identify, as the condition comprises lots of phenotypes. There is no available proof in the published literary works on the clinical result of ES for administration of women BOO. These specific parts of self-management have actually not been reviewed independently and most recommendations are derived from consensus technique. They might help reduce signs and symptoms resulting from BOO yet no metrology of their impact is possible. Extracorporeal magnetic excitement entails the person sitting on a tool that induces consistent PFM contraction and leisure at an established regularity and period by duplicated magnetic excitement of motor nerve fibres. It is proposed that people as a result learn to automatically contract or kick back the PFM, which may improve their capacity to relax their pelvic floor while invalidating [541] Application of electrodes that enable regulated contraction and leisure of the PFMs may theoretically promote the leisure of the exterior sphincter and pelvic flooring but no important evaluation of this treatment in women with BOO has been released. Electromyography alone is not able to properly identify BOO in women, although it might be of use in mix with stress-- flow studies and in differentiation of physiological vs. functional BOO. An alternative urodynamic parameter of area under the detrusor pressure contour throughout voiding (corrected for nullified volume) has been suggested adhering to a possible study of 103 females [534] The authors concluded that this variable seems the most differentiating urodynamic specification for the medical diagnosis of women BOO.Advances In Laparoscopy And Minimally Intrusive Surgery
In addition, the frequency of day-to-day UI changes from 5 to 15%, and it climbs over 15% in females matured over 70 years [14] Although these varieties of occurrence of UI are typically ignored in the professional setting, given that patients often fall short to bring the condition to the attention of their physicians. It is estimated that just one in 4 symptomatic women looks for help for this problem [17] Male urinary incontinence creates unintentional leakage of pee and shows a loss of bladder control. According to studies, it can minimize the quality of life in men dramatically [1] The proportion of clients who undergo surgical treatment for urinary incontinence that are overweight or obese is higher than that of the general population [137] On the other hand, young, elite professional athletes, and women that work-out for health and fitness reveal a high occurrence of UI/SUI [281,302] Utilize a validated and ideal survey as part of the standardised analysis of clients with stress urinary system incontinence.Social Links