Antibiotics and Oral Infections: Usage and Resistance Issues
So, you’ve got an oral infection and you’re thinking, ‘Hey, antibiotics will fix this, right?’ Well, hold on a minute. Antibiotics may not always be the magical cure-all you think they are when it comes to oral infections. In fact, there are some serious issues with their usage and resistance that you need to be aware of.
This short guide will give you the lowdown on the role of antibiotics in oral infections, the factors contributing to antibiotic resistance, alternative treatment options, and strategies for responsible antibiotic use in dentistry.
So, put down that prescription pad for a moment and let’s dive into the world of antibiotics and oral infections.
Key Takeaways
– Antibiotics are effective in treating oral infections by eliminating bacteria and preventing their multiplication and spread.
– Overprescribing antibiotics and inadequate dosage and duration of treatment contribute to antibiotic resistance.
– Alternatives to antibiotic treatment for oral infections include antiseptic mouthwashes, probiotics, and proper oral hygiene practices.
– Responsible antibiotic use in dentistry involves prescribing antibiotics only when necessary, using narrow-spectrum antibiotics, and completing the full course of treatment.
The Role of Antibiotics in Oral Infections
When you have an oral infection, antibiotics can play a crucial role in helping to eliminate the bacteria causing the infection. These medications work by attacking the bacteria directly, preventing them from multiplying and spreading further. By doing so, antibiotics can help to alleviate the symptoms of the infection, such as pain, swelling, and fever. They can also prevent the infection from worsening and spreading to other parts of your mouth or body.
It is important to note that not all oral infections require antibiotics. In some cases, the infection may be mild and can resolve on its own with proper oral hygiene and self-care measures. However, if the infection is severe or if it persists for more than a few days, it’s advisable to seek medical attention. A healthcare professional will be able to evaluate your condition and determine the appropriate course of treatment, which may include antibiotics.
When prescribed antibiotics for an oral infection, it’s crucial to follow the prescribed dosage and duration of treatment. Completing the full course of antibiotics is essential to ensure that all the bacteria causing the infection are eliminated. It’s also important to be aware of the potential side effects of antibiotics and to report any adverse reactions to your healthcare provider.
Factors Contributing to Antibiotic Resistance
To understand the factors contributing to antibiotic resistance in the treatment of oral infections, it’s important for you to recognize the role of improper antibiotic usage. While antibiotics play a crucial role in fighting bacterial infections, their misuse can lead to the development of resistance.
Here are some key factors that contribute to antibiotic resistance:
– Overprescribing antibiotics: Sometimes, antibiotics are prescribed when they aren’t necessary or effective, such as for viral infections like the common cold. This overuse contributes to the development of resistance.
– Inadequate dosage and duration: Not taking antibiotics as prescribed, either by skipping doses or stopping the treatment prematurely, can allow bacteria to survive and develop resistance.
– Self-medication: Taking antibiotics without a prescription or guidance from a healthcare professional can lead to inappropriate usage, contributing to resistance.
Understanding these factors is crucial to combat antibiotic resistance in the treatment of oral infections. It’s essential to ensure proper antibiotic usage, including using them only when necessary, following prescribed dosages and durations, and seeking professional advice rather than self-medicating. By doing so, we can help preserve the effectiveness of antibiotics and prevent the further spread of antibiotic resistance.
Alternatives to Antibiotic Treatment for Oral Infections
Consider non-antibiotic options as viable alternatives for treating oral infections. While antibiotics have been widely used in the past to combat oral infections, their overuse has led to the development of antibiotic resistance. It’s important to explore other treatment options to avoid further contributing to this problem.
One alternative to antibiotic treatment is the use of antiseptic mouthwashes. These mouthwashes contain ingredients such as chlorhexidine and hydrogen peroxide, which have been shown to effectively kill bacteria in the mouth. Using a mouthwash regularly can help reduce the number of bacteria causing the infection and promote healing.
Another non-antibiotic option is the use of probiotics. Probiotics are live bacteria and yeasts that are beneficial to our health. They can help restore the natural balance of bacteria in the mouth and prevent the overgrowth of harmful bacteria. Probiotic lozenges or supplements can be used to introduce these beneficial bacteria into the oral cavity.
In addition, proper oral hygiene practices such as regular brushing and flossing can go a long way in preventing and treating oral infections. Removing plaque and bacteria from the teeth and gums can help reduce the risk of infection and promote oral health.
Strategies for Responsible Antibiotic Use in Dentistry
You can implement strategies for responsible antibiotic use in dentistry to help address the issues of usage and resistance discussed earlier. By following these strategies, you can ensure that antibiotics are used appropriately and effectively in the treatment of oral infections.
– Prescribe antibiotics only when necessary: Carefully evaluate the patient’s condition and symptoms before deciding to prescribe antibiotics. Antibiotics should be reserved for cases where there’s a clear indication of bacterial infection or when non-antibiotic alternatives have been exhausted.
– Use narrow-spectrum antibiotics: Choose antibiotics that target specific bacteria, rather than broad-spectrum antibiotics that can kill a wide range of bacteria. This helps minimize the development of antibiotic resistance.
– Follow recommended dosage and duration: It’s important to prescribe antibiotics at the correct dosage and for the appropriate duration. Completing the full course of antibiotics is crucial, even if symptoms improve, to ensure eradication of the infection.
Future Directions in Managing Oral Infections and Antibiotic Resistance
To effectively address the challenges of managing oral infections and antibiotic resistance, it’s essential to explore future directions in dental care and treatment. As the prevalence of antibiotic-resistant oral infections continues to rise, it’s imperative to develop alternative approaches that can combat these infections effectively. One promising direction is the development of novel antimicrobial agents specifically designed for oral use. Researchers are exploring the use of nanoparticles, probiotics, and natural antimicrobial compounds derived from plants to target oral pathogens without promoting antibiotic resistance.
In addition to developing new antimicrobial agents, another future direction is the implementation of personalized medicine in dental care. This approach involves tailoring treatment plans to an individual’s unique oral microbiome and genetic profile. By understanding the specific bacteria present in a patient’s mouth and their antibiotic resistance patterns, dentists can prescribe targeted therapies that are more effective and reduce the risk of resistance development.
Furthermore, advancements in diagnostic techniques can revolutionize the management of oral infections. Rapid point-of-care tests that can identify the specific pathogens causing an infection and their antibiotic susceptibility can guide treatment decisions. This would enable dentists to prescribe the most appropriate antibiotics, optimizing efficacy while minimizing the risk of resistance.
Lastly, improving oral health education and promoting preventive measures can also play a crucial role in managing oral infections and reducing the need for antibiotics. Encouraging regular dental check-ups, proper oral hygiene practices, and a healthy diet can help prevent the development of infections and reduce the reliance on antibiotics.
Frequently Asked Questions
What Are the Common Symptoms of Oral Infections That May Require Antibiotic Treatment?
If you’re experiencing oral infections that may require antibiotic treatment, there are common symptoms to watch out for. These may include redness, swelling, pain, and pus in the affected area.
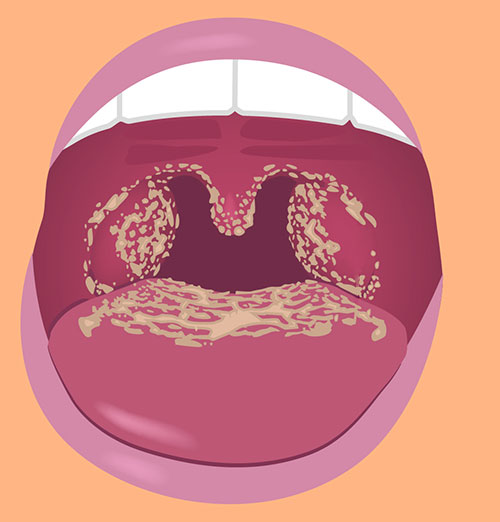
You might also have difficulty eating or speaking, and your breath may have a foul odor.
It’s important to consult a healthcare professional for a proper diagnosis and to determine if antibiotics are necessary for your specific case.
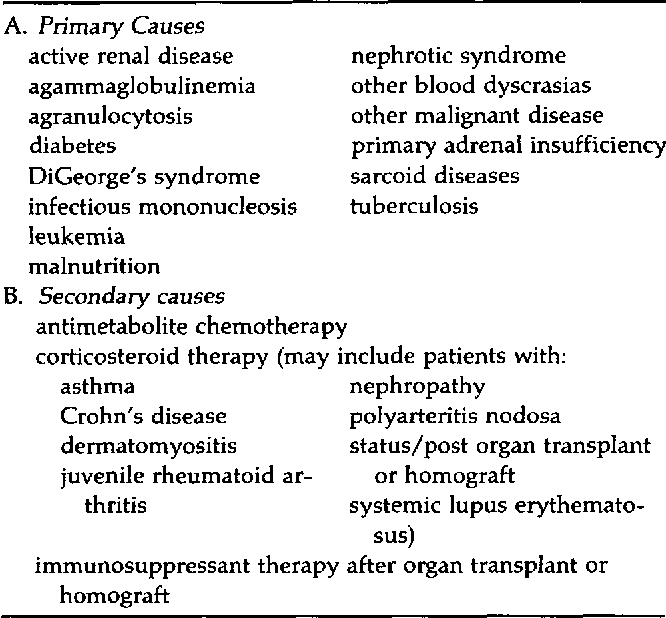
Are There Any Specific Groups of People Who Are More Prone to Developing Antibiotic Resistance in Oral Infections?
You might be wondering if there are certain groups of people who are more likely to develop antibiotic resistance in oral infections.
Well, it’s important to note that anyone can be at risk, but some factors can increase the chances. These include frequent use of antibiotics, inadequate oral hygiene, and underlying health conditions.
It’s crucial to follow proper antibiotic usage guidelines and maintain good oral health practices to reduce the risk of developing resistance.
How Long Does It Typically Take for Antibiotics to Start Improving Symptoms of Oral Infections?
Typically, it takes a few days for antibiotics to start improving the symptoms of oral infections. However, this can vary depending on the severity of the infection and the specific antibiotic being used.
It’s important to follow the prescribed dosage and complete the full course of antibiotics, even if you start feeling better. This helps ensure that the infection is completely eradicated and reduces the risk of antibiotic resistance.
If you have any concerns or questions, it’s always best to consult with your healthcare provider.
Can Over-The-Counter Medications Be Used as an Alternative to Antibiotics for Treating Oral Infections?
Over-the-counter medications can sometimes be used as an alternative to antibiotics for treating oral infections. These medications, such as pain relievers or oral antiseptics, can help to alleviate symptoms and promote healing.
However, it’s important to note that they may not be as effective as antibiotics in treating the underlying infection. If your symptoms worsen or persist, it’s advisable to consult a healthcare professional who can evaluate your condition and determine the appropriate course of treatment.
Are There Any Natural Remedies or Home Remedies That Are Effective in Managing Oral Infections Without the Use of Antibiotics?
There are indeed natural and home remedies that can effectively manage oral infections without the use of antibiotics. These remedies include:
– Rinsing with warm salt water
– Applying a cold compress to reduce swelling
– Using clove oil for pain relief
– Practicing good oral hygiene by brushing and flossing regularly.
It’s important to note that while these remedies can help manage symptoms, they may not be able to fully cure the infection. Therefore, it’s always best to consult with a healthcare professional for proper diagnosis and treatment.
Conclusion
In conclusion, it’s crucial to address the issues of antibiotic usage and resistance in oral infections. Dentistry needs to adopt responsible antibiotic use strategies and explore alternatives to antibiotic treatment.
By doing so, we can minimize the development of antibiotic resistance and ensure effective management of oral infections in the future.
It’s imperative to prioritize the preservation of antibiotics for the benefit of patients and public health.

Welcome to my website! My name is Jett Kirkland, and I am a passionate and dedicated Dental Educator with a strong focus on periodontal treatments, oral infections and care, dental laser therapy, and holistic gum health. With years of experience in the dental field, I am committed to providing valuable information and resources to help individuals achieve optimal oral health.